Poisons
Poison ivy, oak, and sumac are three common and closely related
plants that cause skin rashes. A child who spends a great deal of time
in the woods and fields should know what these plants look like so that
they can be avoided.
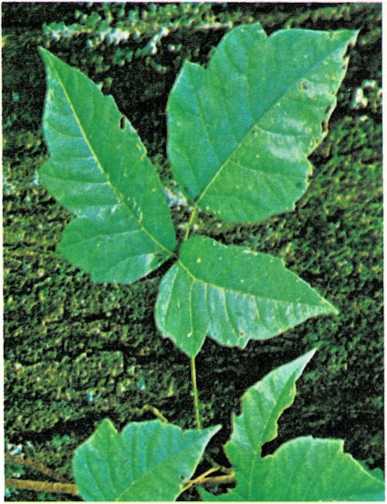
Poison ivy leaves grow in clusters of three, all from the same stem.
The edges of the leaves may be lobed or notched.
Poison ivy grows as a vine or shrub. Some forms of poison ivy are called
poison oak. Poison ivy always has three smooth leaves on one stem. The
leaves are shiny green in summer and turn red or orange in the fall.
Bunches of small, green flowers grow on the main stem close to the
leaves. In autumn and winter, the plant bears clusters of white, waxy
berries.
Poison sumac grows as a shrub or small tree. It has narrow, fernlike
leaves and drooping clusters of white berries.
Poison ivy or poison sumac rash is caused by an irritating oil in the
leaves, flowers, fruit, stem, bark, and roots. Clothing that has come in
contact with poison ivy may irritate the skin just as much as the plants
themselves. Wash or clean the clothing before the child wears it again.
Dogs and cats that have come in contact with the poison ivy may also
cause the rash. Decontaminate your pets by bathing them.
If you think your child has touched poison ivy, immediately wash the
child’s hands and other exposed skin thoroughly with mild soap. Rinse
with plenty of cold water, lather
again, and rinse again. Do not rub too hard and do not use brushes,
sponges, or other rough or harsh materials. Washing with soap removes or
lessens the irritation of the oil.
Poison ivy rash may appear a few hours or a few days after the child
touches the plant. At first the child’s skin itches or burns. Then the
skin becomes inflamed, and it usually develops blisters. Scratching may
cause an infection. Cut the child’s fingernails short. To reduce
itching, soak the rash- covered skin in plain or salt water for 20 to 30
minutes, four or five times daily. Use one level teaspoon of table salt
in one pint (0.5 liter) of water. Apply calamine lotion every two or
three hours. Your doctor may prescribe medicine such as Benadryl® to
reduce itching, [a.mm]
Poisonings and poisons. According to the National Capital Poison
Center, approximately 1,500,000 poisoning cases occur each year. Of all
reported accidental exposures to poisonous substances, 65 per cent
involve children under 6. In addition, an unknown number of poisoning
cases are not reported to poison control centers.
Cases that are reported to poison control centers include exposure to a
wide variety of chemical substances such as cosmetics, plants, cleaning
substances, analgesics, and cold and congestant medications.
Approximately 65 per cent of the incidents are nontoxic, rather than
cases of actual poisoning. Approximately 35 per cent are considered
toxic exposures, or actual poisonings that involve symptoms,
hospitalization, or death.
Factors that affect poisonings. Many factors determine the eventual
outcome for a potentially poisoned child or adult:
The inherent toxicity of the material itself; for example, household
bleach as compared to cyanide.The concentration of the substance ingested (taken in); for example,
bleach drunk straight from the bottle as opposed to a cupful diluted
in a bucket of water.The sensitivity of the child to the substance in question.
The route of the exposure; for example, gasoline spilled on the skin
as opposed to gasoline swallowed during siphoning.The volume or amount ingested.
The time interval since the exposure.
The presence or absence of symptoms.
The number of substances ingested.
The ability to follow instructions from a poison control center or
doctor. Often an appropriate and timely reaction to an incident can
mean the difference between taking care of the problem at home and
going to the emergancy room of a hospital.
How and with what children are poisoned. Cosmetics are the leading
poisonous substance ingested by children under 6. Other leading
poisonous substances, in order, are plants, soaps and detergents, cold
medications (antihistamines or decongestants), analgesics, and vitamins
and minerals.
Aspirin was once a major poison problem with children. However, since
1972, the number of aspirin-related poisoning incidents has declined
steadily. One factor is the Poison Prevention Packaging Act of 1972,
which requires child-resistant packaging. However, other common
household analgesics that are provided in child-resistant packaging show
a slow but steady increase in frequency of ingestions. Unfortunately, no
packaging is absolutely childproof.
Therefore, a number of factors other than child-resistant packaging are
believed to account for the reduction in the number of aspirin
poisonings. The most significant factor is thought to be increased
public awareness of the danger of aspirin. Evidently, parents recognize
the potential danger of aspirin and use and store it properly—out of
sight of curious little minds and out of reach of curious little hands.
The same need for safety precautions applies to all potential poisons in
the home, including acetaminophen, which has replaced aspirin in the
treatment of fever.
Poison prevention. Normal children are inquistive, resourceful, and
almost tireless. They learn by touching, smelling, and tasting the
elements of their environment, and by imitating their parents and other
family members. If an item is attractive in appearance or packaging, is
brightly colored, resembles a food item, or has been consumed by other
family members in the child’s presence, it is a potential poison.
Observing some safety rules, and checking or cleaning
out a few areas of your house, can help protect your child from
poisoning and perhaps help prevent needless pain to both your child and
you.
Safety rules. By following a few simple safety rules, you can
“poison-proof” your home:
Keep hazardous products out of your child’s sight and reach.
Periodically check the entire house and all storage areas for
hazardous materials. Discard any potential poisons that are of
little or no use. Some items commonly involved in poisonings are
furniture polish, lighter fluid, bleach, boric acid, turpentine,
pesticides, antifreeze, drain cleaners, and medicines. Store all
colognes, perfumes, and aftershave lotions (which are all high in
alcohol content) and all “super” glues out of reach.Take extra care during times of family stress or any disturbance of
normal routine (for example, when moving or going on vacation,
during illness, or during holidays).Never refer to medication as candy.
Purchase only those medications and household products that are
available with child-resistant closures. Use these packages as
directed.Never leave alcoholic beverages within your child’s reach. Before
retiring, always discard any alcoholic beverages left in glasses or
cans and empty all ashtrays.Always read the warning labels on hazardous products.
Keep all products in their original containers.
Never put nonedible or hazardous products in cups, pop bottles, or
other containers that would normally be used for food or beverages.Avoid taking medication in the presence of your child.
Promptly dispose of any leftover medication used to treat an acute
illness.Teach your preschoolers not to eat or drink anything unless given to
them by an adult they know.Do not depend on close adult supervision. A child moves quickly, and
with purpose.Be alert for repeat occuiTences. For some unknown reason, a child
involved in an improper exposure or poisoning is likely to attempt a
second ingestion within one year.
“`{=html}
“`
Know the names of all your house plants. Keep potentially toxic
plants out of your child’s reach.Maintain your furnace in good working order. This will help prevent
both natural gas and carbon monoxide poisoning.Keep the telephone number of your physician, hospital emergency
room, and poison control center near your telephone.Seek professional help if your child swallows any nonfood substance.
Keep a one-ounce bottle of syrup of ipecac in your home medicine
chest. This is used to induce vomiting in some poisoning
situations. But do not use syrup of ipecac without professional
advice. In 95 per cent of all cases, syrup of ipecac will cause
vomiting within 30 minutes.Do not use outdated, ineffective, and potentially toxic methods of
inducing vomiting, such as mustard, salt water, or copper sulfate.
In some circumstances, inducing vomiting can have a harmful effect
and may actually create a serious situation from what would have
been a benign ingestion.Do not attempt self-directed home treatment of a poisoned child.
Call the local poison control center.
Guidelines for parents. If a child swallows a nonfood item or is
exposed to toxic fumes, a few basic rules may help to minimize both
physical and emotional trauma to the child and family:
Remain calm.
When possible, estimate the amount ingested or duration of exposure
to the solvent or fumes.Observe the child for symptoms or unusual behavior.
Try to estimate the elapsed time since the ingestion or exposure.
Bring the container to the telephone in case there are questions
about the substance.Call the poison control center.
If the child vomits spontaneously, do not discard the vomit.
If a significant time lapse occurs between ingestion and your
realization of the exposure, save approximately two ounces of each
urine specimen produced. Both vomit and urine may be analyzed if an
emergency room examination is necessary.
Outdoor plants that are poisonous when eaten
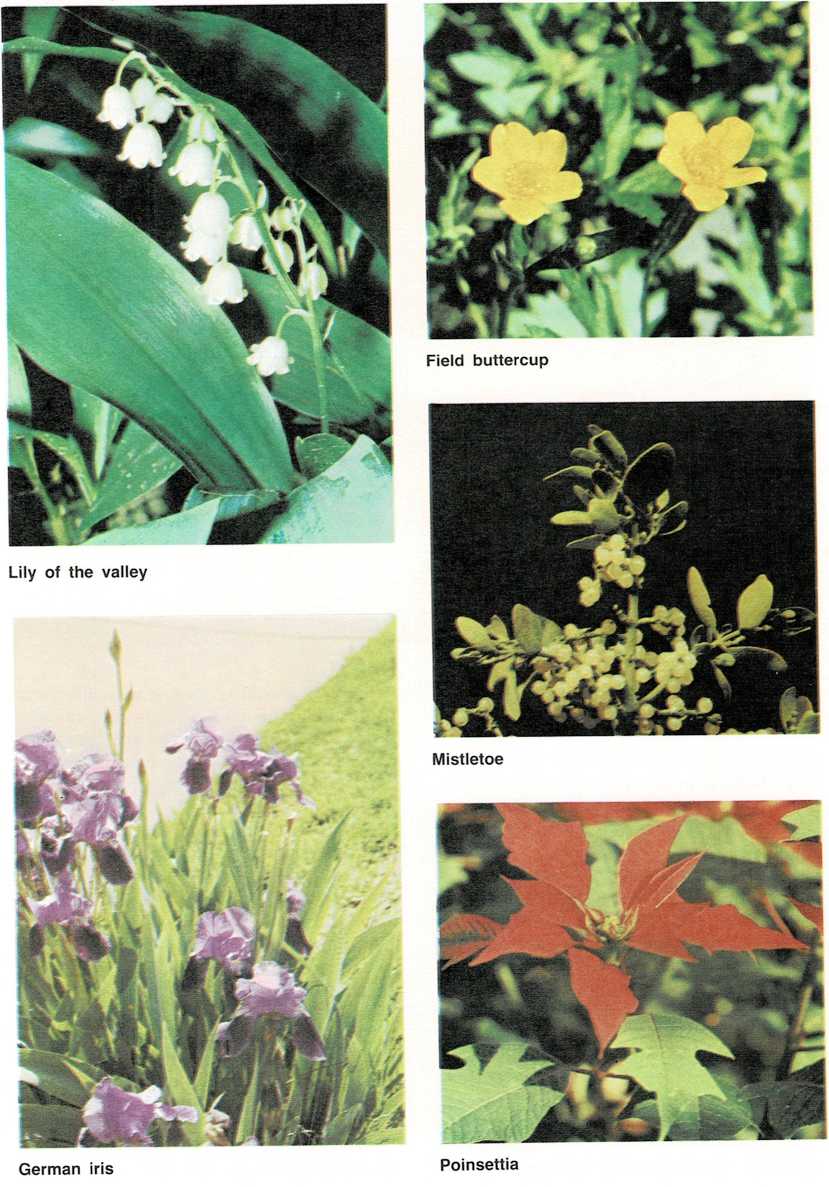
A partial list of toxic plants
(All or some of the parts of these plants are poisonous.)
Aconite Deadly Nightshade Jimson Weed Poinciana
(Monkshood) Delphinium Jonquil (Bird of Paradise)
African Violet Devil’s Ivy Lantana (Red Poinsettia
Sage
Amaryllis Dieffenbachia* or Wild Sage) Poison Hemlock
Azalea (Dumbcane) Lily of the Valley Poison Ivy
–^1^
Begonia Elderberry Lobelia Poison Oak
Black Locust Elephant’s Ear Marijuana Poison Sumac
Black English Ivy Marsh Marigold Pokeweed
Nightshade
Bleeding Heart Flax Milkbush Pothos Plant
(Dutchman\’s- Four-O’Clock Mistletoe Privet
(berries
breeches) Foxglove Moonseed and leaves)
Buckeye Golden Chain Morning Glory Rhododendron
Buttercup (Laburnum) Mother-in-Law Scotch Broom
Caladium Holly Mountain Laurel Shamrock
Calla Horse Chestnut Mushrooms Star of
Bethlehem
Christmas Hyacinth (various wild types) Tobacco
Cherry
Christmas Rose Hydrangea Narcissus Tulip
Chrysanthemum Iris Oak Virginia
Creeper
Crocus, Autumn Jack-in-the-pulpit Oleander Water Hemlock
(Meadow Crocus) Jequirity Bean Pansy (seeds) (Cowbane)
Crown of Thorns (Rosary Pea) Pencil Tree Wisteria
Daffodil Jerusalem Cherry Peony (common) Woody
Nightshade
Daphne Jessamine, Yellow Philodendron* Yew
\’These are the most poisonous house plants.

Cautions. Do not attempt home assessment or home treatment of a
poisoned patient. Do not rely upon a poison antidote/ treatment chart.
Call upon the professional experience of personnel who routinely treat
poisoned patients. Inducing vomiting can worsen the patient’s condition
in certain situations.
For example, you might cause unnecessary injury by inducing vomiting if
the child has ingested certain stimulants, strychnine, an acid or an
alkali, or certain petroleum products (depending upon the nature and
volume ingested), or if the child is unconscious or having a seizure.
Eye contamination. The one situation in which it would be advisable
to begin treatment before seeking professional assistance is in the case
of eye contamination. If damage occurs to the cornea (clear portion of
the eye), it may cause a partial or complete loss of vision. An eye that
has been exposed to
an irritant should be flushed with lukewarm water for 15 minutes. If
more than one adult is present at the time of the exposure, one can
flush the eye while the other contacts a physician, emergency room, or
poison control center.
Several methods of eye washing are possible. The quickest method is to
use a soft stream of lukewarm water from a kitchen faucet. Check the
water temperature several times during the washing, because the
temperature may increase or decrease. Remember to use a gentle stream of
lukewarm water so as not to cause further injury to the contaminated
eye.
The second option is to fill a pitcher with lukewarm water and slowly
pour the water over the eye for 15 minutes. You may need several
pitchers of water to complete a 15- minute flush of the eye.
Any form of eye washing is difficult. If the child is particularly
uncooperative as a result
of pain or fear, the parent has two options. The first would be to step
into the shower with the child, using the shower spray to decontaminate
the eye. Do not waste time removing either the child’s clothes or your
own. Using the shower, however, can be difficult because the force of
the water may contribute to the irritation of the eye.
Second, the parent who is alone and dealing with a combative child may
wish to ask a neighbor for help. But, if you have to work on your own,
wrap the child in a large towel, sheet, blanket, or pillowcase. Keep the
child’s arms inside the wrap. Using a chair to prop your knee up, you
can hold the child on your knee with one hand and, after adjusting the
water temperature, hold the eyelids open with the other hand.
Skin contamination. Another area in which you can do something
before calling for professional assistance is in treating the skin
following exposure to acids, alkalis, petroleum products, or
insecticides. Remove the child’s clothing and bathe the child
thoroughly. Areas that children often wash inadequately include the
fingernails, behind the ears, the groin area, and the scalp. Failure to
wash these areas thoroughly can provide sites for the continued
absorption of the contaminant. Be careful not to splash soap or
contaminated water into the child’s eyes during the bathing process.
Articles made from porous material such as leather cannot be
decontaminated after exposure to most liquid organic substances. Shoes,
belts, watchbands, or other articles made from leather must therefore be
discarded once contaminated.
Warning. Remember, all substances are poisons. There are none that
are not poisons. Only the right dose, administered under the appropriate
circumstances, constitutes a remedy for a poison.
See also Accidents; Bites and stings; Coma; Convulsions; CPR;
Emetics; Food poisoning; Medicine cabinets; Poison ivy, oak, and sumac;
Prescriptions; Vomiting
Symptoms of polio may at first resemble those of a common cold. The
child may have fever, chills, sore throat, headache, severe intestinal
upset, stiff back, muscle spasms in the neck or thighs, or pains and
stiffness in the legs, back, and neck. Some children become paralyzed,
but most do not remain paralyzed permanently. All children with polio
should be under a doctor’s care.
Vaccine has almost eliminated polio in the United States and Canada. The
first vaccine perfected was the inactivated Salk vaccine, in which the
virus is dead but still able to cause production of antibodies. Later, a
live oral vaccine was developed by Albert Sabin. This vaccine contains
the living poliovirus, but the virus has been weakened so that the child
does not catch the disease. Live vaccine provides longer-lasting
immunity, and so children who have been immunized with the Salk vaccine
should also receive oral vaccine.
Giving the oral vaccine is simple. Two drops of the vaccine are dropped
directly into the child’s mouth or onto a small lump of sugar, which is
then fed to the child.
Three types of viruses cause polio, and so a child must be protected
against all three. Type I is the most frequent cause of polio. Type III
is the next most frequent cause, and Type II is the least frequent
cause.
There is an oral vaccine for each of these three types. The doses can be
given separately. These vaccines, called MOPV (monovalent oral
poliovirus vaccine), are most helpful to doctors during an epidemic
caused by a single type of polio.
For routine immunization, most doctors prefer TOPV (trivalent oral
poliovirus vaccine). This vaccine protects against all three types of
polio. It is usually given at 2 and 4 months of age, with a third dose a
year later. If a child is at risk for exposure to polio, an extra dose
of TOPV may be given at 6 months. Many doctors also recommend a fourth
dose of TOPV at 4 to 6 years, or when children enter kindergarten or
first grade, [h.d.r.,] Jr.
