Fever – Fistulas
Fever. The normal oral temperature of the human body is about 98.6°
F. (37° C). A child’s temperature goes up and down a little during each
day, depending on the time of the day and what the child is doing.
Usually, a child’s temperature is slightly lower in the morning and
slightly higher in the afternoon. Exercise, a hot bath, drinking
warm liquids, wearing too much clothing, or merely being out in the sun
may raise a child’s temperature by several tenths of a degree, or even
an entire degree. If your child has a fever after any of these
activities, wait about half an hour before taking the temperature.
A below-normal temperature (around 97° F.; 36° C) may occur at the end
of an illness. As long as the child feels well, do not be concerned.
A fever is present if a child’s temperature is 101° F. (38.3° C) or
higher rectally, 100.2° F. (37° C) orally, or 99° F. (37.2° C) by
armpit. Call your doctor promptly when a fever occurs in an infant under
3 or 4 months of age.
Reducing a fever. If your child has a fever and is uncomfortable,
you may give acetaminophen (aspirin substitute, sold under brand names
such as Liquiprin®, Panadol®, Tempra®, and Tylenol®) in age- appropriate
doses. (Use the table accompanying this article as a guide.) Aspirin has
been linked to Reye’s syndrome and is not recommended for treatment of
children who have a fever. Call your doctor if the acetaminophen does
not control the fever; if the child has a rash, a sore throat, an
earache, is in pain, or appears ill.
Proper dosage of acetaminophen (aspirin substitute)
Avoid overdosage. Check with your doctor before giving more than two
doses.
Age of Amount Frequency
child
6 months .08 cc acetaminophen drops (brand Every 4 to 6 hours
old names: Liquiprin\”, Panadol\”,
Tempra\”, Tylenol\”), or Vz teaspoon
of acetaminophen syrup or elixir
1 year 1.2 cc of acetaminophen drops, or Vz Every 4 to 6 hours
old teaspoon of acetaminophen syrup or
elixir
2 to 3 1.6 cc of acetaminophen drops, or 1 Every 4 to 6 hours
years old teaspoon of acetaminophen syrup or
elixir
4 to 5 3 chewable 80 mg acetaminophen Every 4 to 6 hours
years old tablets, or 1\’/? teaspoons of the
acetaminophen syrup or elixir
How to take a child’s temperature
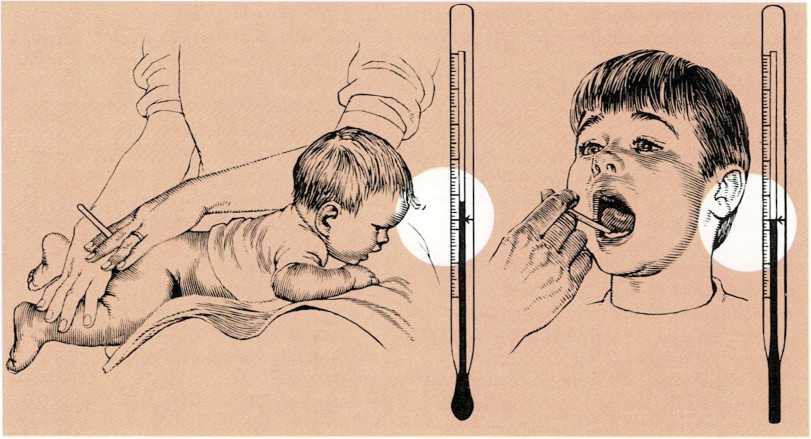
To use a rectal thermometer, lay the child facedown. Insert the bulb
of the thermometer about an inch (2.5 centimeters) into the rectum and
hold it in place gently. Normal rectal temperature is about 99.6° F.
(37.5° C). Use an oral thermometer for older children. Place the bulb
under the tongue. Then the mouth should be kept closed. Normal oral
temperature is about 98.6° F. (37° C).
Some children have convulsions if a fever develops rapidly. If your
child tends to have fever convulsions and is running a high fever, try
to lower the temperature. Give the child acetaminophen in doses
appropriate to age. Also, sponge the skin with cool or lukewarm water.
If the child has a convulsion, call the doctor.
Taking a child’s temperature. The three most common ways of taking a
child’s temperature are by rectum, by mouth, or by armpit. Rectal
temperature registers about a degree higher than oral temperature. The
temperature by armpit registers about a degree lower than oral
temperature. When you report the temperature, tell your doctor how you
took it.
Take the temperature of an infant or young child rectally, using a
rectal thermometer. Check the mercury-filled bulb of the thermometer to
be certain it is not cracked. Then lubricate the tip with petroleum
jelly or cold cream. Lay the child stomach down across your knees.
Gently insert the thermometer about an inch (2.5 centimeters) into
the child’s rectum. Let the thermometer find its own direction. Then,
place your hand on the child’s buttocks and hold the thermometer between
your index finger and middle finger so that the child will not be
injured when moving. Leave the thermometer in place for two or three
minutes.
When the child is a year old, you may want to start taking the
temperature in the armpit. Undress the child so that there are no
clothes between the arm and chest. Use either an oral or a rectal
thermometer. Place the bulb in the armpit and hold the arm against the
side for three minutes.
Temperatures can be taken orally with school-age children. Place the
thermometer under the child’s tongue for three to five minutes. Be sure
the child’s mouth remains closed around the thermometer.
To read a thermometer, hold it at the end opposite the mercury bulb. Do
not hold it by the bulb, because the heat of your fingers may raise the
temperature. Rotate the thermometer until the mercury column appears.
After you have read the temperature, wash
the thermometer with alcohol or cool, soapy water. Hold the thermometer
tightly by the end opposite the bulb. Shake it down by snapping your
wrist. Keep shaking it until the mercury falls, [m.g.]
See also Convulsions; Dehydration
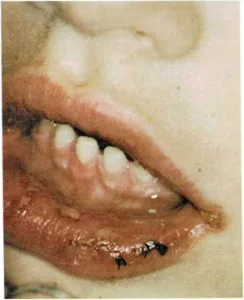
Fever blisters (herpes simplex) usually form on the lips or around
the mouth, but they sometimes form inside the mouth. Fever blisters are
also called cold sores. They are caused by a virus.
Fever blisters often occur along with certain illnesses that cause
fever, such as the common cold or the flu. The blisters also tend to
recur, particularly when the child is subjected to physical or emotional
stress.
The blisters are infectious, so the infected child should have his own
washcloth and towel and should avoid spreading the fluid in the
blisters. The blisters usually dry in three or four days and develop a
crust.
The crust drops off in another three to five days. [m.g.]

A fever blister starts as a patch of red, burning skin. Then
yellowish blisters develop. When these blisters break, they ooze and
form a crust.
Fingernails. See Nail care
First aid. (NOTE: First aid for particular emergencies is described
in separate articles—[Bites and stings; Bleeding; Broken bones;
Burns;] CPR; [Choking; Convulsions; Cuts and scratches;
Dislocation of joint; Electric shock; Frostbite; Nosebleed; Poison ivy,
oak, and sumac; Poisonings and poisons; Shock; Sprain and
strain.)]{.smallcaps}
Most home accidents result in minor injuries, and the needed first aid
is obvious. In more serious cases—severe bleeding, stoppage of
breathing, and poisoning—act quickly, because each second is
important.
First-aid rules. Here are some general steps to follow in giving
first aid: ■ Keep calm.
Have the child lie down.
Check for injuries and do what is immediately needed to stop
bleeding. If breathing has stopped, administer CPR.Call the doctor. If possible, have someone else call the doctor
while you give first aid.Keep the child quiet and continue first-aid treatment until the
doctor arrives.
First-aid kits. To do its job properly in the home, in the family
car, or on a hike through the woods, a first-aid kit should contain
sufficient materials for its probable use. It should be arranged so that
you can quickly remove any item without scrambling the contents of the
entire kit. Individual items should be wrapped separately, so that
unused materials do not become soiled or contaminated.
Surgical supply manufacturers package first-aid kits according to Red
Cross specifications. First-aid kits available in most drugstores and
department stores are not standardized. Examine the contents and
packaging of a kit before buying one.
To meet most emergencies, you should have the following items:
An assortment of adhesive bandage strips Several gauze pads
A roll of adhesive tape
A roll of sterile gauze bandage
A tube of burn ointment
A package of folded, sterile gauze totaling one-half square yard (0.5
square meter) or more. [m.g.]
Fistulas are abnormal tunnels or openings in the body. Generally,
they connect one organ with another organ, or an organ with an abnormal
opening in the skin.
Fistulas occur in three ways:
They may be congenital.
They may result from infection when an abscess ruptures into two
organs, or into an organ and the skin.Or, they may result from an injury that penetrates the body.
Symptoms of fistulas include pain and a discharge of pus or other
matter.
Congenital fistulas. In rare cases, a child is born with a fistula
leading from the navel to either the bowel or bladder. If the bowel is
involved, contents from the intestines ooze from the navel. If the
bladder is involved, urine oozes from the navel. Another fistula that
may be present at birth connects the trachea (windpipe) and the
esophagus (tube that carries food to the stomach). When the baby is
first fed, milk gets into the trachea and causes breathing difficulty.
Infections. Anal fistulas are commonly caused by infections and
abscesses near the rectum. This fistula (called fistula in ano) leads
from the rectum to the anus. Pus, and occasionally excrement, oozes
through the abnormal opening. Regional enteritis (an inflammation of the
intestine) sometimes causes fistulas to develop between loops of the
intestine, from the intestine to the abdominal wall, or from the
intestine to the bladder.
Injuries. An injury, such as a gunshot wound or a fall onto a sharp
object, can harm an artery and a vein and result in an arteriovenous
fistula. Blood runs directly from the artery into the vein, putting an
increased workload on the heart.
If your child has a draining sore on the skin, consult your doctor. Most
fistulas are corrected by surgery. The complexity of the operation
depends on the organs affected. Some, such as the fistula in ano, may
close spontaneously and heal. Sometimes, fistulas are cured by a minor
operation requiring only about a day in the hospital. Those that involve
blood vessels or the trachea are more complicated and require major
operations for correction, [t.m.h]
See also Colitis