Ear, Objects in the – Eczema
Ear, objects in the. If your child says that something is in his or
her ear, do not try to remove the object yourself. The attempt to remove
a foreign object may injure the ear canal or eardrum, or the object may
be pushed farther down the ear canal, making it harder to get out. Call
your doctor. If you cannot reach the doctor, take your child to a
hospital emergency room.
Children are prone to put such things as peas, beans, or corn kernels
into their ears. These vegetables absorb moisture and swell, causing
intense pain and blocking the ear. Paper also swells and causes pain and
blockage. Beads, buttons, and stones that fit into a child’s ears can
cause painful irritation. Sometimes an insect lodges itself in a child’s
ear canal, causes discomfort because of its movement, and frightens the
child with its buzzing. Matches or hairpins may break the skin and cause
a painful infection.
Caution your child never to put anything into the ears. Try to keep
small objects out of the child’s reach, c.r.r
See also Earaches
Earaches are usually caused by infections in the ear canal or middle
and inner ear.
Infections of the ear canal. Excessive wetness (from swimming or
bathing) or trauma (from fingers or foreign objects) can make the ear
canal especially susceptible to infections. Symptoms include pain,
itchiness, and some hearing loss.
Your child’s doctor may treat your child with ear drops containing
antibiotics and corticosteroids. Dry heat from a heating pad and
acetaminophen may also help relieve pain.
Infections of the middle ear (Otitis Media). Otitis Media is one of
the most common problems during childhood. Most ear infections occur
between 6 months and 6 years of age. Children who develop ear infections
early in life have an increased risk of recurrent or chronic infections.
A middle ear infection can easily be diagnosed by the doctor. Oral
antibiotics are usually prescribed for about 10 days. A follow-up ear
examination is necessary to ensure that the infection has been cured.
Fever, vomiting, and diarrhea may accompany a middle ear infection.
Acetaminophen for pain and fever and dry heat to the ear will ease some
of the symptoms, cr.r.
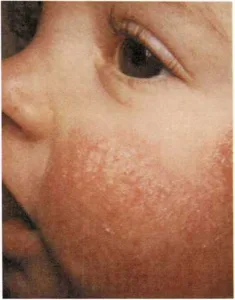
Eczema is a rash that is usually caused by an allergy to a food,
drug, or some irritating substance. Patches of skin become red and itch
persistently. Often the itching is so intense that the child scratches
until the skin breaks and bleeding occurs. Scratching opens the skin, a
colorless fluid oozes from the rash, and the skin becomes thick, coarse,
dry, and scaly. In an infant, the rash appears mainly on the cheeks, and
in the folds of the neck, arms, and sides of the legs. In an older
child, it appears mainly as chronic, thickened areas behind the knees,
in front of the elbows, or in the creases of the neck. In severe cases,
it may spread over the entire body. If you think that your child has
eczema, consult your doctor.
The cause of eczema is often difficult to determine. Your doctor may
suggest eliminating a certain food from the infant’s diet to find out if
that particular food is causing the allergic reaction. In more severe
cases, the doctor may perform skin tests to determine which substances
the child is allergic to. If the doctor is able to discover what is
causing the baby’s eczema, you can sometimes prevent the condition by
removing the offending food from the baby’s diet or by removing the
irritating material from the baby’s surroundings.
Eczema usually begins in infancy. It occurs more often in children with
a family history of allergies. It usually clears completely by the time
the child is 18 to 24 months old. Sometimes, however, it persists
through puberty and into adult life. The skin of a child who has had
severe eczema usually heals without any scars. However, some children
may retain uneven pigmentation of the skin, which is exaggerated by
sunburn. Many children with eczema develop hay fever or asthma as they
get older. A child may also have both eczema and a respiratory allergy
at the same time. If your child has eczema, certain precautions may
reduce the discomfort produced by the rash: ■ Do not let the child’s
skin come into contact with wool or clothing made of synthetic fibers.
Cotton is preferable.
Avoid clothing that causes excessive perspiration.
Avoid irritating soaps, bubble bath, detergents, and excessive
bathing.Keep the fingernails short to lessen damage from scratching.

In infants, eczema usually starts on the cheeks and then spreads to
the folds of the neck and other parts of the baby’s body.
Antihistamines and other drugs may reduce itching, but they should
be used only when prescribed by a doctor.When the skin is red and oozing, wet compresses help relieve itching
and inflammation. Your doctor may also prescribe lotions and
ointments to lessen itching.Keep a baby with eczema clothed, because scratching becomes more
violent when clothes are off.Keep the child occupied to help take the child’s mind off the
itching.
The skin changes caused by eczema make the child’s skin more susceptible
to infection. If a secondary infection occurs, the child may need to be
treated with oral or topical antibiotics, [j.sh]
See also Allergy; Itching