Dehydratation – Dislocation
Dehydration is a condition that results when the water content of
the body drops excessively. It is sometimes accompanied by a loss of
certain body minerals, such as sodium and potassium.
Dehydration is caused by one of two things. The first is an increase in
the loss of water from a child’s body, as may occur with persistent
vomiting, persistent diarrhea, excessive sweating, high fever, severe
burns, or increased urination. The second cause of dehydration is a
decrease in the intake of water, as may occur when a child does not or
cannot drink sufficient fluids for
the body’s normal functions. Sometimes, both factors may cause
dehydration. For example, a child who is vomiting is losing water from
the body. At the same time, the child may not be able to drink any
liquids.
The severity of dehydration depends upon the amount of water and the
amount of minerals lost. Generally, the child’s skin is dry, and the
tongue and the lining of the mouth are parched. Skin may become less
elastic. Babies and young children lose weight. Occasionally, the child
may run a fever of 102° F. (39° C) or higher. In more severe cases of
dehydration, the child may be listless and the eyes may be sunken. The
soft spots (fontanels) in an infant’s head may become depressed.
If your child shows signs of dehydration, call your doctor. If you
cannot reach the doctor, take the child to a hospital. If the diarrhea,
vomiting, or other cause of the dehydration has stopped, give the child
water or cracked ice. If the child can keep this down, then give
frequent small amounts of weak tea, a mixture of half water and half
apple juice, or a carbonated soft drink. A teaspoonful at a time may be
all a small child can take.
The doctor will judge the severity of the dehydration on the basis of
what has caused it and on any signs of dehydration the child has. The
doctor may also examine samples of the child’s blood and urine to
determine if there has been a mineral loss. If the dehydration is not
severe, the doctor may advise oral rehydration. If it is severe, and
especially if there is persistent loss of fluids, the doctor will
probably advise hospitalization and giving fluids intravenously,
[m.g.]
See also Diarrhea; Fever; Soft spots; Urinary disturbances; Vomiting
Diabetes mellitus is a disease in which the body fails to utilize
sugar properly. In children with insulin-dependent Type I diabetes, the
failure generally occurs because of destruction of the cells that
produce insulin, the hormone that enables the body to store and burn
sugar in its normal manner. Diabetes is more common in adults, but it
can occur at any age.
A child with untreated diabetes usually eats a great deal more than is
normal, drinks large quantities of water, and urinates frequently or in
large amounts. A doctor can diagnose the child’s condition by analyzing
the child’s urine and blood. A child who has diabetes will show an
excess of sugar in both blood and urine. If the diagnosis is not made
promptly and treatment begun, the child loses weight rapidly, breathes
deeply and rapidly, is nauseated, vomits, gradually becomes weaker, and
may become drowsy or go into a diabetic coma.
All diabetics should be under a doctor’s care. Although diabetes cannot
be cured, it can be controlled through the use of insulin injections and
diet. Care must be taken to regulate the amount of insulin given,
because too much may lower the blood sugar to a point where the child
may feel unusually hungry or nauseated. The child may perspire and grow
pale, or faint and lose consciousness—sometimes with a convulsion.
This condition is called insulin shock. If a child appears to be
developing insulin shock, offer orange juice or some other food that
contains sugar and promptly call your doctor.
Although the diabetes will be lifelong, it should not interfere with the
child’s psychological and social development. Encourage the child to
participate in the usual childhood activities and to take care of his or
her own dietary and insulin needs. Diabetic children can grow to adult
life able to carry on normal activities, [m.g.]
See also Convulsions; Diets; Drugs; Endocrine glands; Heredity
Diaper rash is so frequent in its mild form that almost every baby
has it sometime. The skin in the diaper area looks red and chafed, and
sometimes there are a few pimples and rough red patches on it. The rash
may spread and the baby may be uncomfortable. Sores of severe diaper
rash on the circumcised penis may result in painful urination.
Severe diaper rash usually results from friction and associated contact
imtants (harsh soaps, detergents, acid stools, or topical medications).
Sweat retention with
excessive heat and moisture are other significant factors.
To treat diaper rash, change wet or soiled diapers frequently. Avoid
using waterproof pants over the diapers, especially on very young babies
or on those with sensitive skin. Rinse the diapers thoroughly after
washing them. The “rinse” cycle of an automatic washing machine usually
rinses the diapers adequately. Disposable diapers may be less irritating
and should be tried.
When your baby’s skin is chafed, let the baby lie without diapers for
several hours after each diaper change. The air will help dry and heal
the skin. Apply a protective preparation, such as zinc oxide paste or a
baby lotion, after the skin has been cleaned with plain water. Your
doctor may want to recommend a preparation.
For severe diaper rash, leave the diapers off for two to four days and
use a fan to circulate the air. If cloth diapers are being used, rinse
the diapers in a vinegar solution—use \’A cup of household vinegar in
the tub of rinse water. Rinse the diapers in this solution after they
have been completely washed and rinsed. After rinsing them in the
vinegar solution, wring the diapers out, or let them go through the
“spin” cycle of an automatic machine, and dry them in the usual way.
Occasionally, diaper rash occurs because enzyme- and bleach-containing
detergents are used in washing the diapers. You can lessen the chances
of this if you use a mild soap and rinse the diapers thoroughly.
If the diaper rash looks like a chemical burn, develops blisters, or
becomes infected, consult the baby’s doctor. Candidiasis (a fungal
infection) and impetigo (a blisterforming skin disease) are fairly
common complications of severe diaper rash. [am.m.]
See also Impetigo
Diarrhea is an intestinal disorder marked by frequent loose, watery
bowel movements. Diarrhea can be serious, especially when it is
accompanied by mucus or blood in the stools, listlessness, failure to
eat, dehydration, vomiting, or fever. If your child’s diarrhea persists
or appears to be serious, call your doctor.
Diarrhea in babies is often caused by problems in feeding. Sometimes the
baby’s formula is not sterilized adequately or is made in incorrect
proportions. Check with your doctor about your formula preparation and
the amounts you are feeding the baby. Sometimes one or two loose stools
may occur when the baby starts eating new solid foods. To help your baby
adjust more easily to new solid foods, cut down on the amount of the
foods and start any new foods slowly. Occasionally, diarrhea may be
caused by a food allergy.
Mild diarrhea may accompany a general infection. Your doctor may
precribe medicine for the general infection. The doctor may also suggest
that you give your child extra fluids (water, diluted formula, or other
liquids) to help replace the fluid lost with the diarrhea. The doctor
will probably tell you to feed the child a bland diet of such foods as
applesauce, cereal, and gelatin.
Sometimes a specific bowel infection causes diarrhea. Be careful to
prevent spreading the infection to other members of your family. Wash
your hands after handling the baby or diapers. Place the diapers in a
covered container and wash them separately from other clothing. Boil the
diapers or iron them to kill germs.
In older children, diarrhea is usually milder, but it occurs for similar
reasons— bowel infection or as part of a general illness. Diarrhea may
also be a symptom of tension or anxiety that occurs at times of stress
or excitement, such as a school examination or a special party. If these
situations frequently cause diarrhea, consider ways to relieve your
child of stress or help avoid too much excitement, [m.g.]
See also Allergy; Dehydration; Food poisoning; Influenza; Sterilizing
Diets. A balanced diet contains all the food elements that a child
needs to grow and stay healthy. A child requires proteins to build body
tissues, fats and carbohydrates for energy, and minerals and vitamins
for growth, maintaining body tissues, and regulating body functions.
Your doctor may prescribe a special diet for your child if the child has
an illness, a
metabolic disorder, a food allergy, or a weight problem. Be certain you
know why the diet is being prescribed and how you can best carry it out.
Here are some questions you may want to ask when the doctor advises a
diet:
■ Is the quantity of food eaten important? If so, how can you keep a
record of what the child eats?
■ How urgent is it to follow the diet closely? In some metabolic
diseases, where the child’s body cannot digest certain component
materials in foods, it is vitally important to follow the dietary
prescription to the letter.
Encourage your child to stay on the diet. If there are choices among
foods, use those the child prefers, especially if the child must remain
on the diet for a long time. Let the child who can understand assume
some responsibility for eating needed foods and avoiding others. Most
children are happy to have this trust placed in them. Older children
often can help plan what they will eat. Helping make such decisions may
give them the incentive to carry them out.
Make diet foods as appealing as you can. For instance, a white cream
soup, served in a colorful bowl or cup with a bright garnish, usually
perks up the appetite of a child on a bland diet.
A child on a diet has to learn to go without eating certain foods, but
try not to put an extra strain on willpower. For example, a child who is
allergic to eggs has to accept the fact that he or she cannot eat eggs
for breakfast even though the rest of the family has eggs. But serve
eggless desserts so that the child can eat the family dessert,
[m.g]
See also Allergy; Anorexia nervosa; Appetite; Nutrition: Overweight;
Underweight; Vitamins
Diphtheria is a severe, contagious disease that causes a membrane to
form in the throat or nose. This membrane may hinder breathing and
eventually cause choking or even death. Diphtheria is caused by
bacteria. Once common, diphtheria is no longer widespread because almost
all children are immunized against it.
Diphtheria usually begins from two to four days after exposure. A child
with diphtheria may have a sore throat, fever, headache,
backache, drowsiness, and vomiting. Yellowish-gray patches may appear on
the throat, the tonsils, or the roof of the mouth. Sometimes the
membrane so completely obstructs the throat that the child cannot
breathe. A doctor may have to perform a tracheotomy (incision into the
windpipe) to get air into the lungs. Call your doctor immediately if you
suspect that your child has diphtheria.
Inoculations of diphtheria toxoid are routinely given in a single shot
along with tetanus (lockjaw) toxoid and pertussis (whooping cough)
vaccine. These inoculations, called DPT shots, are usually begun when
the infant is 2 months old. The last infant DPT shot is given when the
baby is 16 to 18 months of age. As further protection, a DPT booster is
given at 4 to 6 years of age, or when a child enters kindergarten or
first grade.
For nonimmunized children over 6 years of age, two Td shots (combined
tetanus and diphtheria toxoids) are given eight weeks apart. A third
shot a year later completes the immunization.
For continued protection, all immunized children should have a Td
booster shot at 14 to 16 years and at 5- to 10-year intervals during
adult life.
A baby who has received a DPT shot may have a fever and a loss of
appetite, and will be cranky. The area around the injection may be sore
and red. This reaction occurs because of the whooping cough vaccine. To
relieve fever, give acetaminophen in doses appropriate for the baby’s
age. Your baby should feel better the next day. If your baby runs an
excessively high fever or exhibits other abnormal behavior, notify your
doctor. The doctor may wish to modify the immunization schedule,
[h.d.r„] jr.
See also Communicable diseases; Fever; Immunization; Shots; Tetanus;
Whooping cough
Disinfecting. See Sterilizing
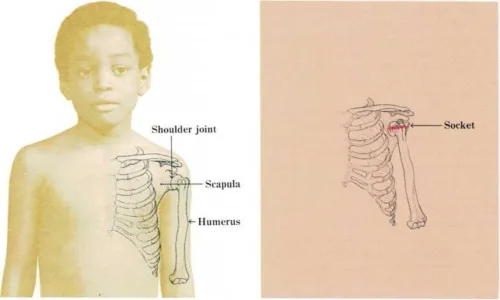
Dislocation of a joint. A joint is dislocated when the two bone ends
that make up the joint become separated and no longer work together.
Most dislocations are caused by injury. They occur most frequently in
the shoulder, elbow, ankle, or finger joints. A
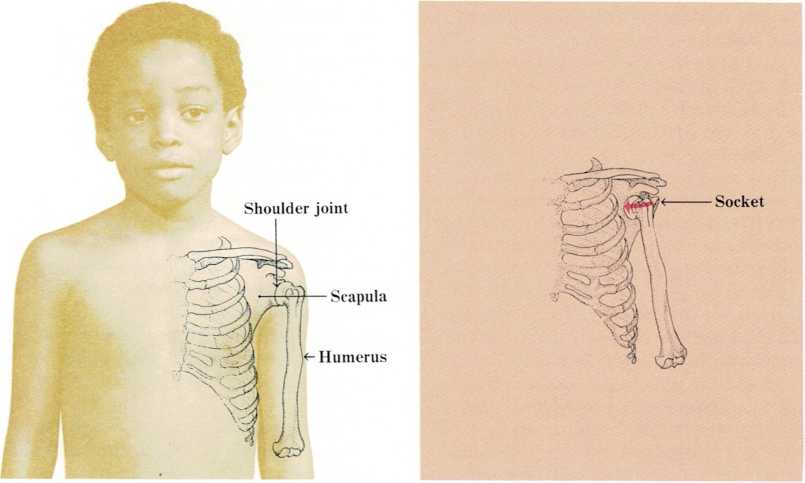
The shoulder joint consists of two bones—the humerus and the
scapula. When the humerus slips out of the socket of the scapula
(right), the shoulder is dislocated and the child experiences
immediate pain.
dislocation causes immediate pain and rapid swelling of the injured
part. There is usually a visible deformity, and the joint cannot be
moved normally. In addition, one of the dislocated bones may be broken.
A joint dislocation is serious and requires immediate medical treatment.
Call a doctor at once and do not move the child. If you cannot reach a
doctor, protect the joint by putting splints on the injured part in the
most comfortable position. Never pull on the bones or attempt to
relocate the joint yourself. After applying the splint, take the child
to a hospital immediately for X-ray examination and proper care. The
child will probably be given an anesthetic, and the doctor will attempt
to gently manipulate the bones of the joint back into their proper
position. Most often this is successful. Rarely, an operation may be
needed to correct the dislocation. The doctor will usually apply a
splint, cast, or brace to protect the healing joint.
Sometimes a joint, usually the shoulder or kneecap, will dislocate
periodically. Surgery is required to correct this condition, v.v.c.
Drowning. See CPR