Broken Bones – Burns
Broken bones, also called fractures, are fairly common during
childhood, particularly among boys. There are several types of
fractures:
In a closed fracture, the broken bone does not cut through the skin.
In an open fracture, a sharp end of the bone sticks through the
skin. Open fractures are considered medical emergencies and are
serious because of the danger of bone infection.A greenstick fracture is a type of closed fracture in which there is
a partial break in a bone. It occurs most frequently in younger
children. Children’s bones are soft and, like a stick of green wood,
may bend and splinter on one side only.In an epiphyseal fracture, the growing ends of the long arm and leg
bones break off or separate. This type of fracture can occur only in
children, and involves the wrist and ankle most frequently.
Some fractures are not immediately apparent. But if the area around an
injury swells, becomes very painful, and is tender to touch, call your
doctor. All obvious fractures require immediate attention. All open
fractures demand emergency treatment in a hospital as soon as possible.
Here are some emergency first-aid measures:
Do not move the injured part, and do not let the child move it.
Moving the sharp, broken ends of a long bone may injure nerves,
blood vessels, and muscles, or cut through the skin. It is
especially important not to move the child if you suspect a back,
neck, or head injury.Encourage the child to lie still and quiet.
Cover open skin wounds with clean or sterile dressings, if possible.
To treat for shock, cover the child with a blanket or extra
clothing.Call the police or fire department for emergency help in getting the
child to a hospital. If no trained emergency help is available, put
a splint on the injured part to prevent further injury when the
child is moved. Do not try to straighten the injured part. Gently
bind it to a board or firm object, such as a tree branch or a piece
of cardboard. If possible, pad the splint by wrapping cloth around
it to avoid pressure on nerves.
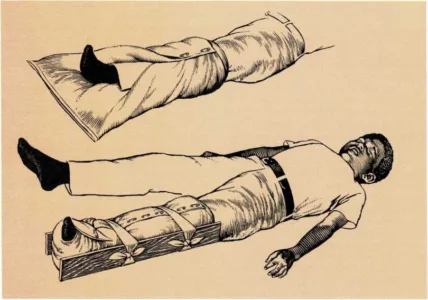
Emergency splinting
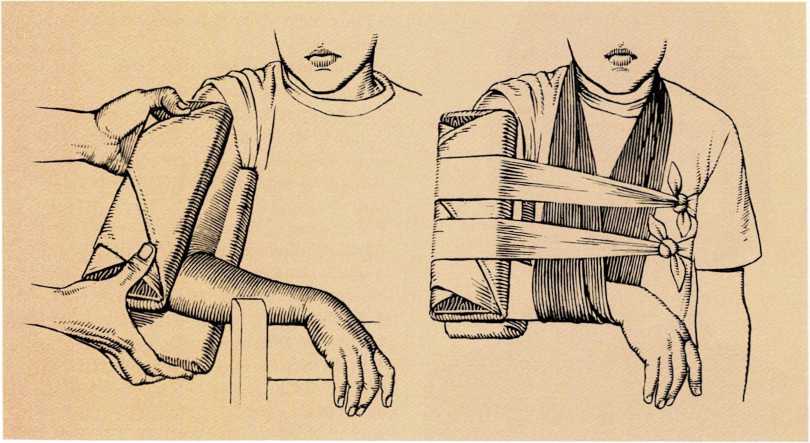
If you must apply a splint to the upper arm, and the arm is bent,
use splints that reach from the armpit to below the elbow. Use a sling
to support the lower arm. Then tie the splints snugly around the
child’s body with strips of cloth.
A pillow splint provides stability for a broken bone in a child’s foot
or ankle.
Gently wrap the pillow around the foot and leg. Next, secure the
pillow with safety pins. Then tie the splints snugly around the child’s
leg with strips of cloth.
If there is a broken bone in the upper arm and the arm is in a bent
position, use a splint that extends from the armpit to below the
elbow.If there is a broken bone in the upper arm and the arm is straight,
use a splint that extends from the armpit to the child’s fingertips.If there is a broken bone in the lower arm, use a splint that
extends from the armpit to the fingertips.For a broken wrist, use a splint that extends from the fingertips to
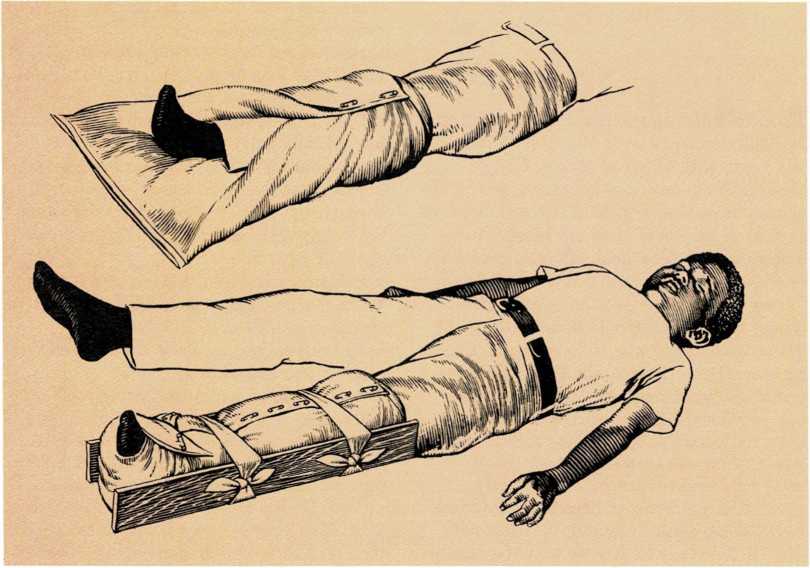
the elbow.For a broken bone in the thigh, use a splint that extends from the
foot to the child’s armpit.If a bone in the lower leg is broken, use a splint that extends from
the foot to the hip.If a bone in the ankle or foot is broken, use a splint that extends
from the foot to the knee.
If it is essential that a child be moved after a back injury, use a wide
board to lift the child so the child’s back will not bend. Also, if it
is essential that you move a child with a suspected neck injury, support
the head firmly so the child’s neck does not move. [jj.c.]
See also Dislocation of joint; shock
Bronchitis is an inflammation of the lining of the bronchial tubes.
It may be caused by allergy, bacteria, a fungus, viruses, or chemical
substances. In most cases, bronchitis is caused by a cold or a lingering
virus infection. Most cases are mild and do not last long. If the
child’s bronchitis lasts for more than a few days, consult your doctor.
The most bothersome symptom of bronchitis is coughing. The cough may be
worse during the night. In severe cases, the cough may start the child
vomiting. Do not give medicine to reduce the cough unless your doctor
prescribes it. Coughing usually rids the bronchial tubes of irritating
material. In severe cases, a chest X ray and other studies may sometimes
be necessary.
Wheezing sometimes occurs in infants and young children with bronchitis,
[m.g.]
See also Allergy; Colds: Coughing;
Humidifying
Bruises (contusions) are injuries that usually do not break the
surface of the skin but are severe enough to cause small blood vessels
to break under the skin. The blood oozes into surrounding tissues.
Swelling and pain occur. The skin may turn red at first, then turn black
and blue as the blood seeps into the tissues. As the blood is gradually
absorbed into the blood system, the skin of the bruised area becomes
yellow and then returns to its normal color. The darker a child’s skin
is, the less noticeable are the color changes.
An ordinary bruise does not need any treatment. But you may reassure and
comfort your child by putting cold cloths on the injured area. Severe
bruises should be treated by a doctor.
Bruises are usually caused by falls, blows, or bumping against sharp or
hard objects. If a child bruises easily, or if bruises appear without
any obvious reason, the child’s blood may not be clotting normally.
Inform your doctor, [m.g.]
See also Blood clotting: Hemophilia
Burns range from minor annoyances to serious injuries that can cause
permanent crippling or even death. Burns are classified according to
degree of severity. A first- degree burn is one that reddens the skin
but does not produce blisters. A second-degree burn reddens the skin and
blisters it. A third-degree burn destroys skin and tissue, and may
penetrate deeply into the body.
Small first- and second-degree burns usually are not serious and require
only minor treatment. But consult your doctor about all second-degree
burns, because an infection may start when a blister breaks. To relieve
pain and decrease injury, put the burned area under cool running water
for a few minutes, pat dry, and cover with sterile gauze or a clean
bandage. If pain continues, apply petroleum jelly and a light gauze
covering. This may relieve the pain. Do not use any greasy substance.
First- and second-degree burns that cover a large area are more serious.
Wrap the child in a clean sheet to avoid infection and take the child to
an emergency room. If this is not immediately possible, immerse the
burned area in cool water (70° F.; 21° C). If you cannot immerse the
burn in water, apply wet compresses. Cool water or a cool compress
lessens pain and helps diminish tissue destruction. Do not apply oily
mixtures, tea poultices, or other home remedies. Consult your doctor at
once.
Never use water on a third-degree burn. Cover the burned area with a
thick, sterile, dry gauze bandage to keep out air. If the burn covers a
large area, wrap the child in a clean sheet. Consult your doctor and get
the child to the hospital at once.
A child who is burned seriously may go into shock. To counteract this,
keep the child lying down and covered with a light blanket. If possible,
raise the legs by resting them on a folded blanket, a pillow, or other
object. If the child is conscious and can swallow, give the child a
drink of water.
If your child is burned by chemicals, immediately wash the affected area
with running water. Use a hose, put the child under a shower, or pour
the water from a bucket or other container. Remove the clothing from the
burned area while continuing to wash with water. Then continue first aid
as for other burns, First aid for burns

For minor burns, run cold water on the burn for several minutes. If
pain continues, apply petroleum jelly and a light gauze dressing over
the burn.

If the burn is a major one and you cannot get the child to a
hospital immediately, immerse the child or the burned part of his body
in cool water.

**For chemical burns, immediately flood the burn with flowing water.
Remove the child’s clothing while rinsing the burn.
See also Accidents; First aid; Shock;
Sunburn