Rash – Roseola
Rash. Since it is difficult to tell a mild, relatively harmless rash
from a serious one, consult a doctor if your child develops a rash which
persists and continues to spread, especially if the child is not feeling
well. Skin color can affect the appearance of a rash. A severe rash on
dark skin may appear milder than it really is. The following are some
common causes of rashes:
Measles—blotchy red rash, cough, conjunctivitis, fever
German measles—rosy rash, low fever, swollen glands in neck and
behind earsRoseola infantum—flat pink rash on the chest, abdomen, and neck
after high feverScarlet fever—a rash that looks like a sunburn with goose pimples,
usually associated with a sore throat and feverChicken pox—separate, raised pimples, some of which blister, then
break and crustEczema—patches of itchy, rough red skin
Hives—itchy white welts on red skin
Ringworm—circular, rough patches
Impetigo—blisterlike sores that crust
Prickly heat—raised, red, pinpoint spots, usually in the groin and
neck foldsDiaper rash—red, chafed-looking skin
Poison ivy—blisters and inflammation accompanied by much itching
Rocky Mountain spotted fever—purple spots on palms and soles, with
headache and fever following a tick bite. Take your child to the
doctor at once if you suspect Rocky Mountain spotted fever.
[a.m.m.]
Reye’s syndrome is an uncommon disease that occurs in children from
a few years of age to adolescence. It involves the liver and brain and
often follows an attack of chicken pox or influenza.
A child may be recovering from a mild respiratory infection when
suddenly there is persistent vomiting. This is followed by behavioral
changes consisting of lethargy alternating with irritability,
hyperactivity, and hallucinations. Should your child show such symptoms,
call your doctor immediately. If the diagnosis is Reye’s syndrome, the
patient needs emergency treatment and should be taken to a hospital
equipped to give all the help necessary.
This disease is named for Dr. R. D. K. Reye, who, with Australian
colleagues, first described cases of it in 1963. Its cause is still
uncertain and proper treatment is unclear. The general aim is to reduce
the brain swelling and restore normal liver metabolism. Most patients
also have a high blood ammonia level which must be lowered, [si.
k]
Rh factor is a chemical substance that most people have in their
blood. It gets its
name from rhesus monkeys, in whose red blood cells it was first
discovered. The Rh factor is inherited. If the factor is present in a
child’s blood, the blood is Rh-positive. If the factor is absent, the
blood is Rh-nega- tive. Both types of blood are normal and healthy, but
they do not always mix safely.
For example, if a child with Rh-negative blood receives a transfusion of
Rh-positive blood, the Rh-positive blood may cause production of
antibodies that attack the child’s normal red blood cells. The child may
become seriously ill or even die. Hospital technicians test a child’s
blood to determine the Rh factor before transfusions are given.
It is also important to know the Rh factor when a woman is pregnant, or
when a husband and wife are planning to have a baby. The baby of an
Rh-negative mother and an Rh-positive father may be Rh-positive or
Rh-negative. If the baby is Rh-negative, there is no problem. But if the
baby is Rh- positive, the blood may cause the mother’s Rh-negative blood
to produce antibodies against the Rh factor. These antibodies may then
return to the baby’s blood and destroy the red blood cells. The
infant—commonly called an “Rh baby”—may die before birth or may be
born with mild to severe jaundice and anemia. The opposite condition—
an Rh-positive mother and an Rh-negative baby—does not cause trouble.
Once the blood of an Rh-negative woman starts to produce antibodies, the
level of antibodies becomes progressively stronger with each Rh-positive
pregnancy. Generally, an Rh-negative woman with an Rh-positive husband
can have two or three healthy Rh- positive babies because her antibody
production may be slow enough that these first babies escape its
effects. But if an Rh-nega- tive woman has ever had a transfusion of
Rh-positive blood, her blood may already contain antibodies that can
react dangerously with her baby’s Rh-positive blood.
With correct and immediate treatment, a seriously affected Rh baby can
usually make a good recovery and be normal. Doctors can detect Rh
incompatibilities by simple blood tests that measure the level of
antibodies. If the level rises threateningly, the doctor may induce
early labor so that the baby can be delivered before the level of
antibodies is
dangerously high. Sometimes, exchange transfusions must be given to the
baby immediately after birth. These transfusions replace the baby’s
blood with fresh blood. In rare cases, transfusions of blood have been
given to unborn infants. Transfused blood must be Rh-negative, because
Rh-positive blood would be destroyed by the antibodies in the baby’s
system.
For protection in future pregnancies, a vaccine is available to prevent
the production of antibodies in the mother’s blood. It may be given to a
mother with Rh-negative blood within 72 hours after delivery or
miscarriage of an Rh-positive baby.
The best protection against the heartbreak of an Rh baby is competent
prenatal care. A doctor can take proper measures to have on hand the
equipment, typed blood, and other materials for treating the Rh
condition. [k>.]
See also Anemia; Blood type; .Jaundice
Rheumatic fever is a disease that follows an untreated infection by
group A beta hemolytic streptococcal bacteria. The infection is usually
a strep throat. Rheumatic fever, now an uncommon disease, usually first
strikes between the ages of 5 and 15.
Symptoms of rheumatic fever generally appear within two to five weeks
after the strep infection has cleared up. Chorea (St. Vitus’s Dance),
with uncontrollable twitching of muscles, may be one of the first
symptoms. Or, the child may have vague pains in the muscles. (However,
the great majority of children with muscle pains in their legs at night
do not have rheumatic fever.) These pains may become intense. The joints
in the child’s legs and arms may become red, painful, and swollen. The
child may also have a fever and a skin rash. At the same time, the heart
and the heart valves usually become inflamed. This inflammation causes a
heart murmur.
Rheumatic fever can cause permanent damage to the child’s heart, but not
always. When permanent damage does occur, it usually results from
inflammation of either or both of the valves on the left side of the
heart. As the inflammation lessens, a scar forms on the valve. This scar
prevents the valve from opening and closing properly.
The damaged valve may allow blood to leak back when the heart contracts.
Or, the valve may become so puckered and shrunken that the child’s heart
can scarcely force blood through it.
If you suspect that your child has rheumatic fever, consult your doctor.
The doctor will likely advise hospitalization of the child. Bed rest
during the severe phase of the disease is essential for a child with
rheumatic fever. Convalescence at home may be necessary for a time. The
doctor will probably prescribe a gradual increase of physical activity
as well as acetaminophen, and, in special cases, steroid medications to
relieve the symptoms.
A child who has had rheumatic fever is not immune to it. The child is
susceptible to recurring attacks. Each additional attack may damage the
heart valves. Eventually, the valves may become so scarred that an
operation is necessary. Strep infections are a greater threat to a child
who has already had rheumatic fever. To protect the child, the doctor
will prescribe a long-term program to prevent a strep infection. The
child may receive a daily oral dose of a sulfa drug or an antibiotic
such as penicillin, or may have an injection in the buttocks of a long-
acting antibiotic once a month. This protective treatment may be
continued until the child is about 21 or even older.
The best way to fight rheumatic fever is to prevent it. Call your doctor
if your child has a sore throat with a fever, a persistent sore throat,
or an extremely sore throat. The doctor may want to take a throat
culture, because this is the only way to identify the beta hemolytic
streptococcus. If the doctor finds this streptococcus, antibiotics will
be prescribed immediately. This treatment will continue until another
throat culture shows that the infection has cleared up. Fortunately,
most sore throats are not strep throats, [m.g.]
See also Arthritis; Chorea; Cramps; Growing pains: Heart murmur;
Strep throat
Rickets is a bone disease caused by a metabolic disturbance in the
body. Some children with rickets do not get enough vitamin D in their
diets. Others have an inherited
disability that prevents absorption of vitamin D from food. Rickets is
extremely rare in the United States and Canada.
In most cases rickets occurs before the child is 3 years old. The bones
of the child do not calcify (harden) adequately. They are so soft that
they can bend out of shape. Bumps can also develop on the bones. Severe
rickets causes bowed legs, short stature, and deformed skull, rib,
backbone, and pelvic bones. Bone damage can be corrected if it is not
too severe. If rickets is not corrected, the bones may eventually harden
and leave the child misshapen, [mg.]
Ringworm is a contagious skin disease caused by fungus. It may be
itchy. Ringworm of the body usually appears as scaly, circular, pinkish
patches. As a patch grows larger, the center clears and the eruption
looks like a ring. Ringworm of the scalp is characterized by round, red,
scaly patches in which hairs break off close to the scalp. Ringworm
infection of the feet, commonly called athlete’s foot, usually appears
in the
webs of skin between the toes. It usually produces cracked, itchy,
tender skin. Blisters and scaly skin may appear on the soles and sides
of the feet. If you think your child has ringworm, call your doctor.
Antifungal drugs can clear up the disease.
Ringworm may be spread by contact with infected people, infected dogs or
cats, or infected brushes, combs, and furniture. Children who have
ringworm should use their own combs, brushes, washcloths, towels, and
other personal articles. They should be cautioned against scratching the
infected areas, because if they scratch, they may spread ringworm to
other parts of the body, [a.m.m]
Roseola infantum is a disease characterized by a rash and a fever.
Doctors believe that it is probably caused by a virus. Roseola infantum
usually affects children between 6 months and 3 years of age.
Roseola infantum usually begins with a fever of 103° to 105° F. (39.4° C
to 40.6° C). After three to five days, the child’s temperature suddenly
drops to normal or below.
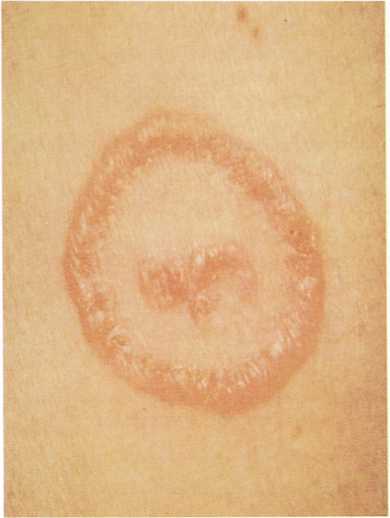
Small, circular patches of pink skin are characteristic of ringworm of
the body.
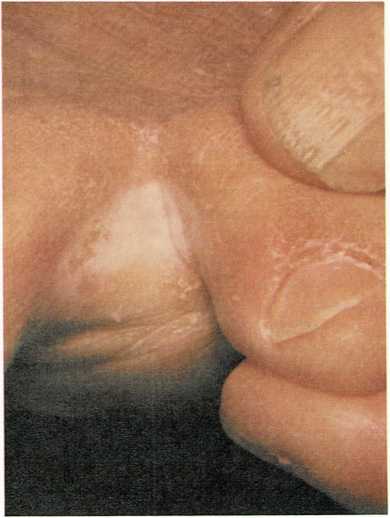
Athlete’s foot usually produces cracked, itchy, tender skin between
the toes.
Then a rash of small, pink, flat spots appears on the chest, abdomen,
and neck. Only rarely does it spread to the child’s face, arms, and
legs. The rash may last a few hours or one or two days. One attack
usually provides permanent immunity.
Call the doctor if you suspect that your child has roseola infantum. The
,doctor will probably tell you to give the child acetaminophen to bring
down the fever and liquids to prevent dehydration. You do not have to
isolate a child with roseola infantum. [h.hr.,] Jr.
Rubella. See German measles

