Immunization – Itching
Immunization. The purpose of immunization is to protect a child from
disease. Immunization generally starts when a child is 2 months old. A
child’s first vaccine combines immunization against diphtheria, tetanus
(lockjaw), and pertussis (whooping cough). The combined shot is called
DPT vaccine. Oral polio vaccine is given separately, usually at the same
time as the DPT shots. MMR, a combined vaccine against measles, mumps,
and rubella (German measles), may be given when the child is 15 months
old. Hemophilus influenzae vaccine may be given at 18 months.
Combined doses. Combined doses of DPT and MMR early in life set up
immunity against common childhood diseases. Combined doses save the
doctor’s time, as well as time and money for parents—and the child
undergoes less pain and anxiety.
A combined dose is no harder on a child medically than single ones.
Reactions are rarely severe. If your child does react— with swelling
or reddening at the site of the injection, or with a fever, unusual
sleepiness, or a convulsion—after a dose of triple antigens, tell the
doctor before the next dose is given. The doctor may omit the whooping
cough vaccine at that time.
Early immunization. Immunization is begun young so that a child will
become immune as soon as possible. Inherited immunity from an immune
mother cannot be depended upon to protect a child from whooping cough,
polio, tetanus, and diphtheria. Immunity to these diseases is not
achieved until more than a month after the last of the primary doses,
and the doses are given about two months apart. Even with an early
start, the child is several months old before becoming immune.
But perhaps the most important reason for early immunization is to
prevent whooping cough, which is a most serious and some-
Immunization schedule
+—————+—————————+————————–+
| Age | Disease | Date given |
+===============+===========================+==========================+
| 2 months | Diphtheria, whooping | |
| | cough, and tetanus; (DPT) | |
| | polio (OPV) | |
+—————+—————————+————————–+
| 4 months | Diphtheria, whooping | |
| | cough, and tetanus; polio | |
+—————+—————————+————————–+
| 6 months | Diphtheria, whooping | |
| | cough, and tetanus; | |
| | polio* | |
+—————+—————————+————————–+
| 15 months | Measles, mumps, and | |
| | German measles (MMR) | |
+—————+—————————+————————–+
| 18 months | Diphtheria, whooping | |
| | cough, and tetanus; | |
| | polio\” | |
| | | |
| | Hemophilus influenzae, | |
| | type B (HIB) | |
+—————+—————————+————————–+
| 4 to 6 | Diphtheria, whooping | |
| years | cough, and tetanus | |
| | booster; polio booster | |
+—————+—————————+————————–+
| 14 to 16 | Diphtheria and tetanus | |
| years | booster (dT) | |
+—————+—————————+————————–+
| Every 10 | Diphtheria and tetanus | |
| years | booster (dT) | |
| thereafter | | |
+—————+—————————+————————–+
| Special | Cholera | |
| im | | |
| munizations | | |
| | | |
| (When your | | |
| doctor | | |
| advises) | | |
+—————+—————————+————————–+
| | Infectious henatitis | |
| | (Henatitis | |
+—————+—————————+————————–+
| | Influenza . | |
+—————+—————————+————————–+
| | Plaoue | |
+—————+—————————+————————–+
| | Pneumococcal | |
+—————+—————————+————————–+
| | Rabies _ | |
+—————+—————————+————————–+
| | Tvohoid Fever | |
+—————+—————————+————————–+
| | Yellow Fever. | |
+—————+—————————+————————–+
| | | |
+—————+—————————+————————–+
*The American Academy of Pediatrics considers this third immunization
for polio to be optional and generally desirable only in areas where
polio is present.
**May be given simultaneously with the MMR vaccine at 15 months.
times fatal disease during the Booster doses. A periodic
first year of life. Measles is also booster dose is routine procedure
a dangerous disease, and during an for maintaining immunization
outbreak, 6-month-old babies may be against diphtheria, whooping cough,
inoculated, with another shot given tetanus, and polio. Also, a dose of
at 15 months of age. tetanus toxoid may be given to an
immunized child
who has been bitten by an animal, has stepped on a nail, or has a burn
contaminated by soil.
Special vaccinations. Special immunization is needed by children who
are going to travel to places where they may be exposed to diseases
other than those for which they have had vaccinations, or where food and
water may be contaminated. Immunizations against diphtheria, whooping
cough, tetanus, and polio should also be brought up to date.
[m.g.]
See also Bites and stings; Communicable diseases; Diphtheria; German
measles; Measles; Poliomyelitis; Shots; Tetanus; Whooping cough
Impetigo is a contagious skin infection that most often affects
children. It is caused by bacteria (staphylococci or streptococci) that
grow on the skin. It may develop from infected insect bites.
Small, blisterlike sores containing pus develop on the skin. These sores
usually open and a thick, honey-colored crust devel
ops over them. The crust drops off in from four to six days.
To lessen chances of spreading infection, a child with impetigo should
keep fingers away from infected parts and avoid scratching. Separate
washcloth, towels, and toys should be used. Bed linen should be changed
daily. The child should not return to school until the condition has
improved with treatment prescribed by your doctor.
If your baby shows symptoms of impetigo, consult your doctor. Babies
with impetigo should be watched carefully. Rarely, the bacteria may get
into the blood and cause blood poisoning, [a.m.m.]
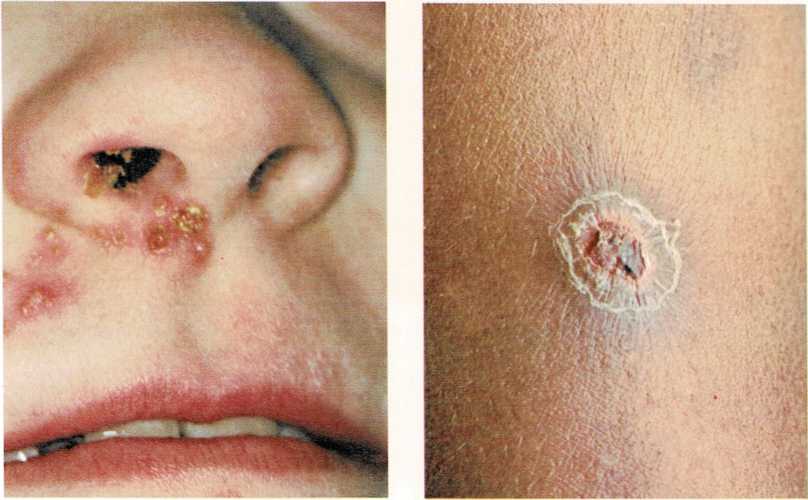
Small blisters are the first sign of impetigo. These blisters break,
releasing pus, which forms a crust. The coloring of the crust may
vary, depending on the skin coloring. A darker skin produces a darker
crust.
Infantile paralysis. See Poliomyelitis**
Infectious mononucleosis. See Mononucleosis
Influenza (flu or grippe) is an infectious disease caused by a
virus. There are several
types of influenza, caused by different viruses that are present in
secretions and other discharges from the nose and mouth of an infected
person.
Doctors believe that influenza is spread mainly by coughing and
sneezing.
Usually, influenza lasts a relatively short time. Symptoms may include:
a chill, aching muscles (especially in the back), and a fever as high as
105° to 106° F. (40.6° to 41° C). The child usually has a hacking cough
and may complain of a sore throat. The symptoms of influenza last
several days and then gradually fade if no complications develop.
Afterward, the child may lack energy for a time.
If you suspect that your child has influenza, call your doctor. Keep the
child’s diet light—mainly liquids. Do not give the child aspirin,
since it is believed that aspirin might induce Reye’s syndrome.
The most serious problem with influenza is the complications that may
develop. The disease leaves children feeling weak. They are also
susceptible to middle-ear infections, pneumonia, and inflammation of the
brain.
There is no drug that cures all the various types of influenza;
antibiotics may be helpful in the treatment of secondary infections.
Antiviral drugs have been found to be effective in the prevention and
treatment of influenza A virus strains. They are not, however, normally
used except with high-risk patients or with patients suffering from
severe influenza A virus illness.
Vaccines for preventing influenza are available, but their protection
lasts only a short time, possibly only six months to a year. Also, no
one vaccine can immunize against all types of influenza. In rare cases,
children react to the vaccine (for example, fever and other symptoms of
influenza). Consequently, doctors do not generally recommend the
vaccines unless an epidemic of influenza appears to be developing.
Children with such diseases as tuberculosis, diabetes, muscular
dystrophy, heart disease, and lung disease should receive the vaccine if
an epidemic is likely, [h.d.r.,] Jr.
Inguinal hernia. See Hernia
Inoculations. See Immunization; Shots
Itching is a symptom of many diseases and conditions. Cool, moist
compresses may help relieve itching, but you must find the cause before
you determine the treatment. Here are some causes of itching:
Allergies including hives and eczema cause severe and, at times,
uncontrollable itching. Sometimes, a child who has completely
recovered from eczema may continue to scratch when going to bed,
when undressed, or when emotionally upset.Hay fever may cause itching of the eyes, ears, nose, throat, or the
roof of the mouth.Pinworms cause intense itching around the anus, usually during the
night.Athlete’s foot (ringworm of the feet) causes itching between the
child’s toes.Mosquito, flea, and bedbug bites can cause itching.
Chicken pox causes itching when it is forming blisters.
Scabies causes intense itching in the area of the bites.
Poison ivy, oak, or sumac causes a burning itch, blistering, and
crusting, [j.s.h.]
See also **Allergy; Chicken pox; Pinworms; Poison ivy, oak, and sumac;
Ringworm

