CPR – Croup
CPR (cardiopulmonary resuscitation) is an emergency procedure that
combines artificial respiration with manual heart (cardiac) massage.
Instructions for both parts of the procedure are provided in this
article.
CPR is used to open the passage from the lungs to the mouth, to move air
in and out of the lungs by making the chest alternately expand and
contract, and to force blood from the heart to other parts of the body
by compressing the heart periodically. Using this procedure can prevent
irreversible brain damage or death if the breathing and heartbeat have
stopped.
If possible, CPR should be performed by someone who has been trained in
the technique. Training is often available through community agencies.
If you have not had CPR training yourself, the following explanation
will help you become familiar with the procedure.
CPR is also more easily performed by two people. If possible, have one
person administer artificial respiration and the other person perform
cardiac massage.
When a child’s breathing stops for any
reason, quickly begin artificial respiration and check the child’s
pulse. If no pulse can be felt, apply CPR immediately (both artificial
respiration and heart massage) while someone else calls the Emergency
Medical Services (usually 911; check your local emergency number).
If the child’s breathing has stopped because of drowning, lay the child
stomach down on a flat surface, turn the child’s head to one side, and
press down on the back before you start CPR. This clears water from the
child’s throat and trachea (windpipe) so air can pass freely.
Turn the child faceup, turn the head to one side, and clear the mouth of
any foreign object. Then put your hand under the child’s neck and tilt
the head back.
Artificial respiration. Begin CPR with mouth-to-mouth resuscitation.
This provides positive air pressure to inflate a child’s lungs
immediately. It also enables the person administering CPR to judge the
volume, pressure, and timing needed to inflate the lungs. When
administering mouth-to-mouth resuscitation to a child, take relatively
shallow breaths to match the child’s own small breaths. Continue until
the child’s normal breathing resumes or until professional help arrives.
When handling an infant, be careful that you do not exaggerate the
backward position of the head tilt. An infant’s neck is so pliable that
forceful backward tilting might block the child’s breathing passages
instead of opening them.
Do not pinch the nose of an infant who is not breathing. Cover both the
mouth and the nose with your mouth and breathe slowly (1 to 1.3 seconds
between breaths) to make the chest rise. For a small child, pinch the
nose, cover the mouth with your mouth, and breathe as for an infant.
Check for pulse periodically. In an infant, the pulse is determined by
feeling on the inside of the upper arm midway between the elbow and the
shoulder. For children older than 1 year, locate the carotid pulse by
sliding your fingertips down the side of the Adam’s apple (voice box)
into the groove next to it. If you cannot find a pulse, you will need to
alternate artificial respiration with chest compressions.
How to give mouth-to-mouth artificial respiration
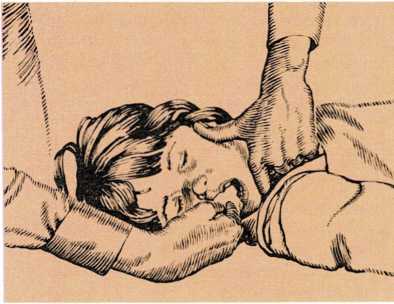
1. The victim should be lying on a firm surface with the head turned
to one side. Use your fingers to remove any foreign object from the
child’s mouth.

2. Place one hand under the victim’s neck and the other hand on the
forehead. Then tilt the head back. If the head is not tilted back, the
tongue may block the throat.
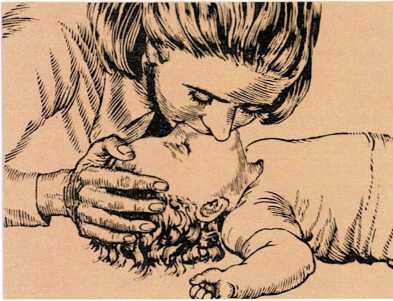
3. If the victim is a small child or infant, take a shallow breath.
Cover both the nose and mouth of the victim with your mouth. Blow into
the mouth and nose every three seconds.
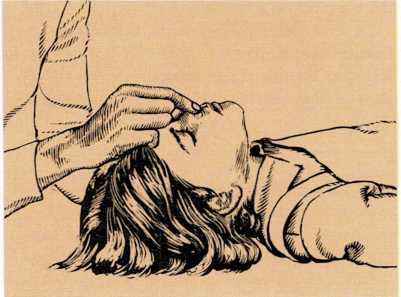
4. If the victim is a large child or adult, pinch the nostrils shut
with the thumb and index finger of the hand pressing on the forehead.
This will prevent any leakage of air.

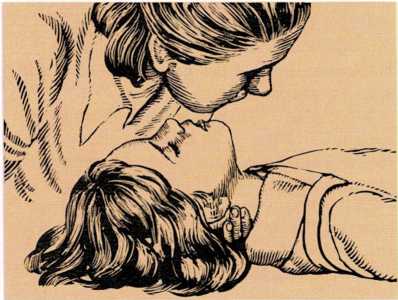
5. Take a deep breath and cover the victim’s mouth with your mouth.
Blow into the victim’s mouth. A large child or adult needs about one
breath every five seconds.
6. Watch the victim’s chest. When it rises, turn your head and
listen for a return rush of air. When the victim has finished
breathing out, repeat step 3, or steps 4 and 5.
Cardiac massage. In infants and small children, only one hand is
used for chest compressions. For an infant, you may slip the other hand
under the back to provide firm support. Use only the tips of the index
and middle fingers to compress an infant’s chest at the sternum
(breastbone), pressing down one finger’s width below the line between
the nipples. Be sure not to depress the tip of the sternum. Depress the
chest at least 100 times a minute.
For small children, use only the heel of one hand on the sternum where
the bottom of the two halves of the ribcage meet in the middle of the
chest. Depress the sternum 80 to 100 times a minute.
For both infants and small children, pause after every fifth chest
compression and give the child a breath.
Cradle cap is a scalp condition that may occur during the first few
months of a baby’s life. Whitish scales form on the baby’s scalp and
then flake off. If the condition is not treated, the scales form a
heavier crust that is yellowish and greasy. When cradle cap reaches this
stage, the scalp may look a little red and irritated, and a rash may
develop on the baby’s face and chest, and in the armpits.
The best way to prevent cradle cap is to shampoo the baby’s scalp
thoroughly (including the soft spots) at the beginning of each bath. Use
soap and water and a washcloth.
If your baby has already developed cradle cap, repeat the following
steps once or twice a day:
Comb the scalp with a fine-toothed comb.
Gently scrub the scalp with a mild soap. ■ Dry the scalp thoroughly.
Apply several drops of baby oil to the scalp and rub it in
thoroughly.
If the condition does not improve in a few days, consult the baby’s
doctor, [a.m.m.]
Cramp is the sudden painful contraction of a muscle or group of
muscles. A cramp is caused by some unusual event irritating
muscle tissue. Although cramps may occur in any part of the body, leg
and stomach cramps are the most common.
Leg cramps usually occur at night, after the child goes to bed. The
child may be awakened by painful cramps in the calf and thigh muscles.
You can usually relieve the pain by massaging the cramped muscles.
Muscle cramping may be caused by sudden overstretching or overactivity
of muscles. The most common cause of muscular leg cramps in a child,
however, is flat feet. The abnormal arch of the foot strains the leg
muscles, and they develop cramps during rest periods. Consult your
doctor if your child has leg cramps frequently.
Abdominal and intestinal cramps may occur in girls during the menstrual
period. Applying heat and using acetaminophen may help relieve pain.
Abdominal and intestinal cramps may also be caused by appendicitis, an
ulcer, food poisoning, or emotional upset. If the cramps last longer
than 24 hours or are accompanied by severe vomiting, call the doctor,
[jj.c.]
See also Charley horse; Colic; Colitis; Elat feet; Food poisoning;
Growing pains; Menstruation
Crib death (Sudden Infant Death Syndrome or SIDS) is the sudden and
unexpected death of an infant, usually while asleep. Ongoing research
has not yet established the cause or causes of death. It is estimated
that more than 8,000 babies die in the United States each year because
of crib death.
Some stricken infants are reported to have had a mild respiratory
infection a week or two earlier. But most infants are apparently in
excellent health just before death. Some even had a satisfactory
physical examination on the day they died.
Crib death is the most frequent cause of death in infants between 2
weeks and 9 months of age, with most deaths occurring between 2 and 3
months of age. Most deaths occur between midnight and 9 A.M. Boys are
affected more often than girls, and infants of low birth weight are more
likely to be affected than those of average or high
birth weight. While crib deaths may occur at any time during the year,
they are more frequent in colder months.
Parents who have had a baby die from crib death often feel responsible
for the death. Their guilt feelings, while natural, are not supported by
facts. There is no way in which crib deaths can be predicted or
prevented. These infants do not suffocate in their bedclothing. And they
do not die because of poor care. Crib deaths can occur to infants of the
most capable parents.
Parents who have had one child die from crib death usually worry about
the possibility of a second baby dying in the same manner. There is an
increased risk, which is considered to be five times greater than the
risk of the general population. Parents who have experienced a SIDS
death in their family may have concerns about their subsequent children.
These parents should discuss their concerns with their doctor, who may
arrange for an evaluation of the new baby.
Contact the National Sudden Infant Death Syndrome Foundation, 8240
Professional Place, 2 Metro Plaza, Suite 205, Landover, Maryland 20785
for information on crib deaths, [m.g.]
Cross-eye (strabismus). Many babies’ eyes “drift” during the first
few months of life. One eye or the other will turn in occasionally,
making the child look cross-eyed. Let your doctor decide if the
condition of your child’s eyes requires attention. If the baby’s eyes
are not straight most of the time by one month or all the time by 3
months, the doctor will probably suggest that the infant be referred for
a special eye examination.
If treatment for cross-eye is started early, chances of correcting the
cause of the disorder are excellent. The doctor may recommend
eyeglasses. The doctor may recommend that the child wear an eye patch
over the good eye to make the crossed eye work harder to develop good
vision. If these corrective measures fail to straighten the child’s
eyes, a surgical operation may be necessary.
If crossed eyes are not corrected, the child may lose the sight of the
crossed eye. [r.o.s.]
See also Eye health
Croup is a respiratory illness characterized by a hoarse, barking
cough and tightness in the child’s breathing. A child with croup makes a
harsh, wheezing noise when taking a breath (stridor). This may be the
result of an inflammation of the larynx (voice box) or the bronchi (air
passages) leading to the lungs.
Spasmodic croup, in which the child does not have a fever, is the most
common and mildest form of croup. It comes upon the child suddenly at
night and may be repeated for several nights. Humidify the child’s room
with a cool-mist humidifier or vaporizer. If neither is available,
create a steamroom in your bathroom by running a hot bath or shower.
Stay with your child to make sure the child does not get into the hot
water. Twenty minutes in a steamy bathroom should greatly ease the
child’s symptoms. Giving the child plenty of water and fruit juice will
also help. When you put your child back to bed, elevate the child’s head
and shoulders to make breathing easier.
Laryngobronchitis is a form of croup that is caused by a viral
infection. This type of croup is accompanied by fever and other coldlike
symptoms. The hoarse, barking cough and tight breathing can occur both
day and night. Steam or mist will not adequately treat this kind of
croup.
If your child has difficulty breathing, appears very ill, or does not
improve with cool mist, take the child to the doctor as soon as
possible. If you cannot reach the doctor, take the child to a hospital
emergency room. [m.g.]

